FEBRUARY 8 — Malaysia has made undeniable progress in healthcare infrastructure over the past few decades. New hospitals continue to be built, specialist centres are expanding and advanced medical equipment is becoming more accessible across the country. These developments reflect strong national commitment to public health.
Yet despite this growth, public hospitals remain overcrowded, healthcare workers are overstretched and patients often face long waiting times even for basic services. This situation raises a critical question. Do we truly need more hospitals or do we need smarter ways to keep people from needing them in the first place?
The healthcare system today is largely reactive. Many patients seek medical attention only when symptoms become severe enough to disrupt daily life. By the time they arrive at hospitals, conditions that could have been prevented or managed earlier such as diabetes complications, hypertension, infected wounds or chronic respiratory diseases, have already worsened. As a result, hospitals are burdened with cases that require intensive treatment, higher costs and longer recovery times. This reactive approach is unsustainable, both financially and socially.
Prevention, early detection and continuous monitoring must therefore become the foundation of Malaysia’s healthcare strategy. A large proportion of hospital admissions are linked to non-communicable diseases, which account for significant healthcare expenditure and long-term disability. Many of these conditions are manageable through lifestyle changes, regular monitoring and timely intervention. However, the current system still relies heavily on hospital-based care rather than empowering individuals to manage their health proactively within their communities.
This is where smarter healthcare solutions play a crucial role, particularly those driven by biomedical engineering, digital health and community-based care models. Technologies such as wearable health monitors, paper-based diagnostic sensors, home glucose testing kits and telemedicine platforms allow health issues to be detected early before they escalate into emergencies. These solutions are often far more affordable than inpatient treatment and can be deployed widely, including in rural or underserved areas where access to hospitals is limited.

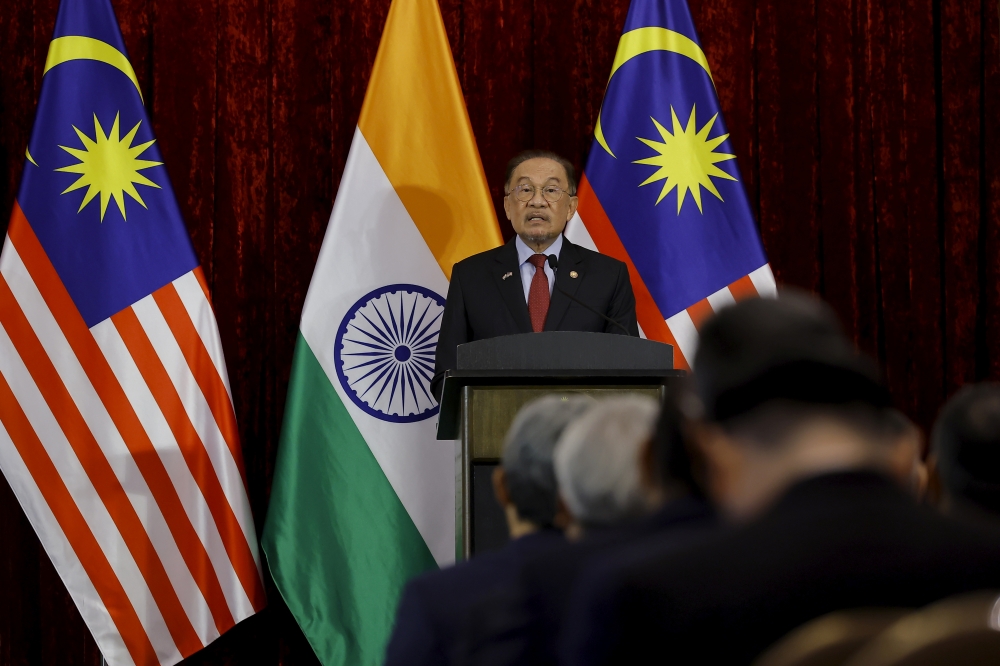
A doctor attends to a patient during a consultation at a clinic in Shah Alam, Selangor, on Nov 2, 2020. — Picture by Yusof Mat Isa
Malaysia already has strong foundations to support this shift. Smartphone usage is widespread, internet connectivity continues to improve and there is a growing pool of skilled engineers, clinicians and researchers. Together, these factors create an ideal environment for preventive healthcare innovation. Yet adoption remains slow. Fragmented healthcare systems, limited integration between engineering solutions and clinical workflows and a culture that prioritises treatment over prevention continue to hinder progress.
Keeping people out of hospitals does not mean denying care. Instead, it means shifting appropriate care closer to where people live. Community clinics, mobile health units and home-based monitoring systems can manage many conditions that do not require specialised hospital facilities. For instance, regular monitoring of wound pH and temperature can help detect early signs of infection, preventing complications that would otherwise require emergency admission. Similarly, remote consultations can be used for follow-up appointments, reducing unnecessary travel, long waiting times and pressure on hospital staff.
A smarter healthcare system also benefits healthcare workers. Doctors and nurses in Malaysia frequently experience burnout due to heavy workloads and constant patient overflow. By reducing avoidable hospital visits, healthcare professionals can focus their time and expertise on patients who genuinely require advanced or specialised care. This improves efficiency, enhances job satisfaction and ultimately raises the quality of care provided.
However, technology alone is not the solution. Strong policy support, public education and interdisciplinary collaboration are equally important. Engineers must work closely with clinicians to design tools that are practical, reliable and aligned with real clinical needs, rather than solutions that look impressive but are difficult to use in practice. Policymakers must invest not only in hospital construction but also in preventive health programmes, digital infrastructure and clear regulatory pathways that encourage innovation while safeguarding patient safety and data privacy.
Most importantly, the public must be empowered to take ownership of their health. Preventive healthcare can only succeed when individuals understand the value of early action. Public awareness campaigns, community engagement initiatives and health education programmes should emphasise that seeking help early is not a sign of weakness but a responsible step towards long-term wellbeing.
Malaysia therefore must redefine how success in healthcare is measured. Instead of focusing solely on the number of hospitals built or beds added, success should be reflected in reduced hospital admissions, healthier ageing populations and fewer preventable complications. Achieving this shift requires courage, investment and collaboration across sectors but the long-term benefits are undeniable.
The future of Malaysian healthcare should not exist only within hospital walls. It should be present in homes, communities and everyday life, quietly preventing illness, identifying risks early and supporting people to stay healthy for longer. That is the smarter and more sustainable way forward.
* Zareen Nadra Mohd Nasir is a final year student at the Department of Biomedical Engineering, Faculty of Engineering, Universiti Malaya.
* This is the personal opinion of the writer or publication and does not necessarily represent the views of Malay Mail.